The HoT study is for patients with low risk thyroid cancer. Low risk means that the cancer is small or medium sized, has not spread to other organs and there is a very high chance of curing it.
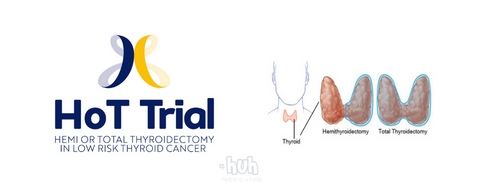
The thyroid is a gland in the throat that produces chemicals (hormones) to regulate certain functions of the body. For many years the most common treatment for thyroid cancer was to remove all of the thyroid gland (total thyroidectomy). This carries greater risks then removing half of the gland (hemi thyroidectomy). Following this procedure patients need to take thyroid hormone tablets and often calcium and Vitamin D tablets for the rest of their lives. This is necessary to make up for the lost function of the thyroid gland. But doctors and researchers now think that it may not always be necessary to remove all of the thyroid gland. Instead they would remove only the part which is affected by cancer (hemi thyroidectomy). As some of the thyroid gland is left behind, patients may not need life-long hormone tablets and vitamin D and calcium tablets. The HoT study has been set up by two surgeons in Edinburgh and London to investigate if it is as safe and effective to remove only that part of the thyroid in which the cancer has been found.
The project is funded by the National Institute of Health Research Health Technology Assessment (NIHR HTA). The trial is being coordinated by the Cancer Research UK & UCL Cancer Trials Centre and plans to recruit 456 patients from 30 hospitals across the UK over a period of four years.
In Aberdeen the study is led by Mr Aspinall, Consultant Endocrine and General Surgeon. He told us why this is an important study: “This randomised controlled trial will hopefully provide high level evidence on whether less extensive surgery is safe and effective in low risk thyroid cancer. Up to now we have only had evidence to answer this question from retrospective (i.e. looking back at results from previous operations) research studies, which are less accurate and reliable than randomised prospective studies. As removing all the thyroid gland carries greater risks of complications which can affect patients’ long-term quality of life, this is an important research question, and I’m delighted that we will be recruiting patients from Aberdeen to take part in this study.